Meningitis- Overview
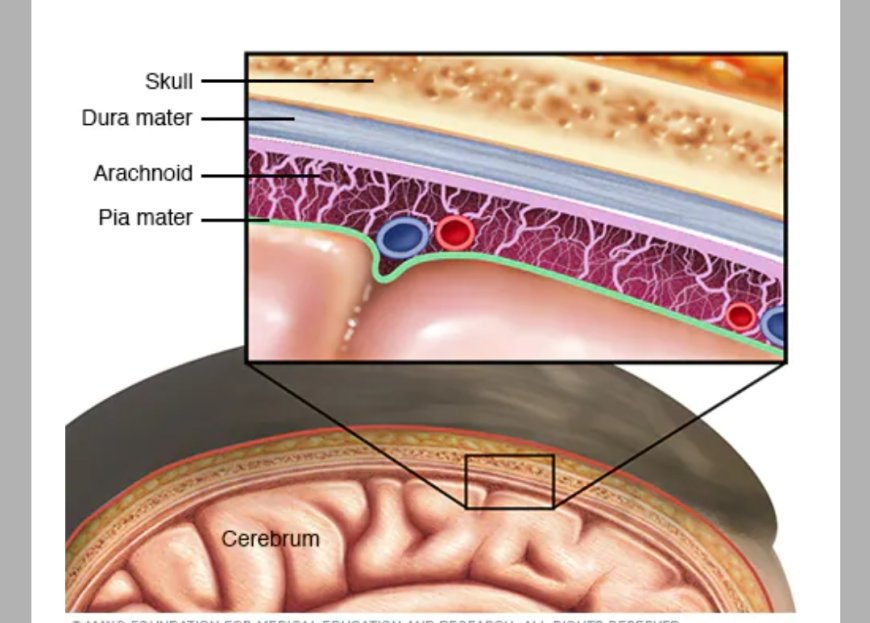
Meningitis Meningitis is an infection and inflammation of the fluid and three membranes (meninges) protecting the brain and spinal cord. The tough outer membrane is called the dura mater, and the delicate inner layer is the pia mater.
Overview
Meningitis is an infection and inflammation of the fluid and membranes surrounding the brain and spinal cord. These membranes are called meninges. The inflammation from meningitis typically triggers symptoms such as headache, fever and a stiff neck. Most cases of meningitis in the United States are caused by a viral infection. But bacteria, parasites and fungi also can cause it. Some cases of meningitis improve without treatment in a few weeks. Others can cause death and require emergency antibiotic treatment.
Seek immediate medical care if you suspect that you or someone in your family has meningitis. Early treatment of bacterial meningitis can prevent serious complications.
Symptoms
Early meningitis symptoms may be similar to the flu. Symptoms may develop over several hours or over a few days.
Possible symptoms in anyone older than the age of 2 years include:
Sudden high fever.
Stiff neck.
Severe headache.
Nausea or vomiting.
Confusion or trouble concentrating.
Seizures.
Sleepiness or trouble waking.
Sensitivity to light.
No appetite or thirst.
Skin rash in some cases, such as in meningococcal meningitis.
Signs in newborns
Newborns and infants may show these signs:
High fever.
Constant crying.
Being very sleepy or irritable.
Trouble waking from sleep.
Being inactive or sluggish.
Not waking to eat.
Poor feeding.
Vomiting.
A bulge in the soft spot on top of the baby's head.
Stiffness in the body and neck.
Infants with meningitis may be hard to comfort. They may even cry harder when held.
When to see a doctor
Seek immediate medical care if you or someone in your family has meningitis symptoms, such as:
Fever.
Severe headache that doesn't go away.
Confusion.
Vomiting.
Stiff neck.
Bacterial meningitis is serious and can cause death within days without prompt antibiotic treatment. Delayed treatment also increases the risk of permanent brain damage.
It's also important to talk to your health care provider if you've been exposed to someone with meningitis. That may include a family member or someone you live or work with. You may need to take medicines to prevent getting an infection.
Causes
Other meningitis causes
Meningitis also can result from noninfectious causes. They include chemical reactions, drug allergies, some types of cancer and inflammatory diseases such as sarcoidosis.
Risk factors
Risk factors for meningitis include:
Skipping vaccinations. Risk rises for anyone who hasn't completed the recommended childhood or adult vaccination schedule.
Age. Most cases of viral meningitis occur in children younger than age 5 years. Bacterial meningitis is common in those under age 20.
Living in a community setting. College students living in dormitories, personnel on military bases, and children in boarding schools and child care facilities are at greater risk of meningococcal meningitis. This is probably because the bacterium is spread through the respiratory route, and spreads quickly through large groups.
Pregnancy. Pregnancy increases the risk of an infection caused by listeria bacteria, which also may cause meningitis. The infection increases the risk of miscarriage, stillbirth and premature delivery.
Weakened immune system. AIDS, alcohol use disorder, diabetes, use of immunosuppressant drugs and other factors that affect your immune system increase the risk of meningitis. Having a spleen removed also increases risk. People without a spleen should get vaccinated to lower the risk.
Complications
Meningitis complications can be severe. The longer you or your child has the disease without treatment, the greater the risk of seizures and permanent neurological damage, including:
Hearing loss.
Memory problems.
Learning disabilities.
Brain damage.
Trouble walking.
Seizures.
Kidney failure.
Shock.
Death.
With prompt treatment, even people with severe meningitis can have good recovery.
Prevention
Common bacteria or viruses that can cause meningitis can spread through coughing, sneezing, kissing, or sharing eating utensils, a toothbrush or a cigarette.
These steps can help prevent meningitis:
Wash your hands. Careful hand-washing helps prevent the spread of germs. Teach children to wash their hands often, especially before eating and after using the toilet, spending time in a crowded public place or petting animals. Show them how to thoroughly wash and rinse their hands.
Practice good hygiene. Don't share drinks, foods, straws, eating utensils, lip balms or toothbrushes with anyone else. Teach children and teens to avoid sharing these items too.
Stay healthy. Maintain your immune system by getting enough rest, exercising regularly, and eating a healthy diet with plenty of fresh fruits, vegetables and whole grains.
Cover your mouth. When you need to cough or sneeze, be sure to cover your mouth and nose.
If you're pregnant, take care with food. Reduce your risk of a listeria infection by cooking meat, including hot dogs and deli meat, to 165 degrees Fahrenheit (74 degrees Celsius). Avoid cheeses made from unpasteurized milk. Choose cheeses that are clearly labeled as being made with pasteurized milk.
Vaccinations
Some forms of bacterial meningitis are preventable with the following vaccinations:
Haemophilus influenzae type b vaccine (Hib). The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) recommend this vaccine for children starting at about 2 months of age. The vaccine also is recommended for some adults, including those who have sickle cell disease or AIDS and those who don't have a spleen.
Pneumococcal conjugate vaccine (PCV15 or PCV20). These vaccines are part of the CDC recommended routine vaccination schedule for children younger than 2 years. They also are part of the recommended vaccine schedule for children age 2 through 18 who are at high risk of pneumococcal disease.
Pneumococcal polysaccharide vaccine (PPSV23). Older children and adults who need protection from pneumococcal bacteria may receive this vaccine. The CDC recommends the PPSV23 vaccine for all adults older than 65; for younger adults and children age 2 and older who have weak immune systems or chronic illnesses such as heart disease, diabetes or sickle cell anemia; and for anyone who doesn't have a spleen.
Meningococcal conjugate vaccine (MenACWY). The CDC recommends that a single dose be given to children ages 11 to 12, with a booster shot given at age 16. If the vaccine is first given
between ages 13 and 15, the booster is recommended between ages 16 and 18. If the first shot is given at age 16 or older, no booster is necessary.
This vaccine also can be given to children between the ages of 2 months and 10 years who are at high risk of bacterial meningitis or who have been exposed to someone with the disease. It's also used to vaccinate healthy but previously unvaccinated people who have been exposed in outbreaks.
Serogroup B meningococcal vaccine (MenB). The CDC recommends this vaccine for adults and children 10 years and older who are at increased risk of meningococcal disease. They include adults and children with sickle cell disease, who have a damaged spleen or who have had their spleen removed. They also include people with the rare immune disorder called complement component deficiency or who take certain medicines. This vaccine may be recommended if you're in a population that's having an outbreak of serogroup B meningococcal disease.
https://www.mayoclinic.org/diseases-conditions/meningitis/symptoms-causes/syc-20350508
What's Your Reaction?